The concept of antigens and neoantigens.
The concept of antigens and antibodies
An antigen refers to a substance that can induce or guide the immune system to produce antibodies. Antigens are generally a small segment of the antigen-producing substance. When the antigen-producing substance is broken down (by enzymatic and acidic digestion) by immune cells, the antigen is generated from the indigestible antigen-producing substance. Antigens derived from normal cells of the body are called self-antigens. Antigens originating from foreign pathogens are called foreign antigens. Antigens derived from mutated cells, tumor cells, cancer cells, and their derivatives are collectively referred to as neoantigens or new antigens, which can also be referred to as mutated antigens, tumor antigens, and cancer antigens respectively. Because there are many types of mutated cells, tumor cells, and cancer cells, and they vary from person to person, it is necessary to classify the antigens in mutated cells, tumor cells, and cancer cells into self-antigens and new antigens when comparing or controlling for oneself.
Individual-specific self-antigens
Individual-specific x'k'y
Antibodies are immune response products produced in response to antigen stimulation. Antigens are generally a fragment of the antigen-producing substance. Therefore, multiple polyclonal antibodies can be produced from the antigen-producing substance.
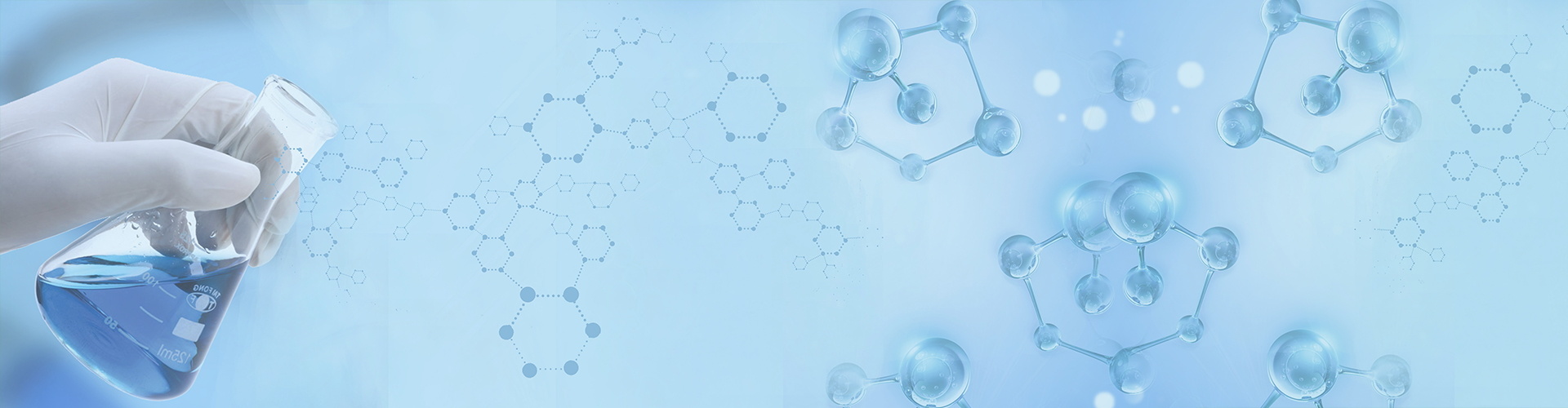
The genome DNA of a normal human cell is about 1 million genes long, with approximately 35,000 genes distributed in the non-coding regions of DNA (about 965,000 genes long). The human body is a genomic ecosystem that grows, develops, and evolves from a single genome. Each person's genome is different, and therefore, their genomic ecosystems are also different. In this genomic ecosystem, there are about 10 trillion cells. When all cells have normal genomes, the human body is healthy and disease-free; when some cells undergo mutations, they may die, be eliminated by the immune system, or escape the immune system's destruction. Mutated cells that escape immune system destruction continue to grow, and after forming a certain number of populations, they cause discomfort or disease in the body. Compared to normal cells, these populations of mutated cells have new antigens. Therefore, new antigens are genomic mutations that escape immune evasion. These genomic mutations are commonly found in populations of mutated cells.
When mutated cells occur in tissues and express cancer genes, precancerous cells are formed, and precancerous cells undergo rapid clonal growth to form benign tumors. The characteristic of benign tumors is that the genomes of precancerous cells are stable, without a population of cancer cells that have genomic instability. Of course, cancer cells arise from further mutations of precancerous cells, so the growth of benign tumors continuously increases the chances of cancer cell occurrence.
When mutated cells occur in the bone marrow or immune cells and express cancer genes, leukemia caused by precancerous cells is formed. If precancerous cells continue to mutate into cancer cells, blood cancer is formed.
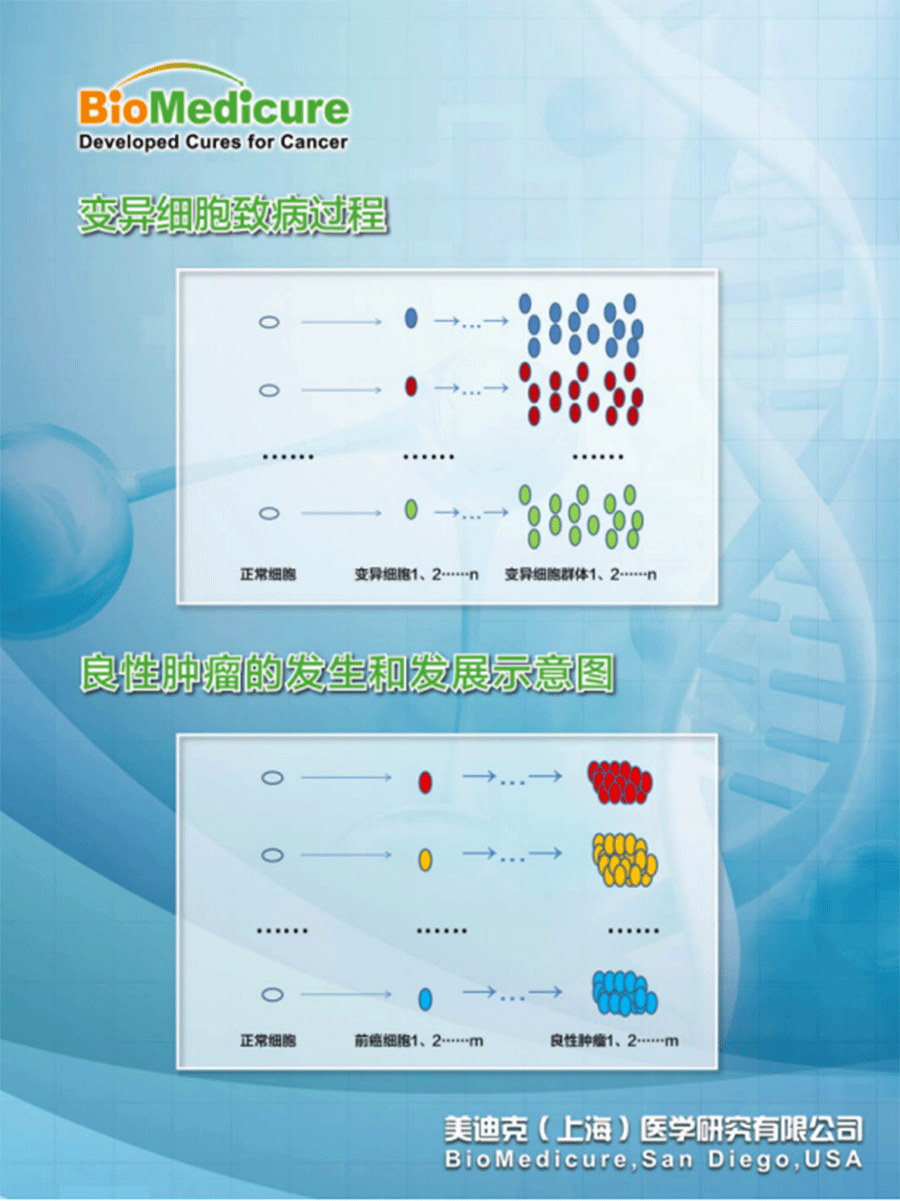
Therefore, cancer is a malignant lesion characterized by the presence of cancer cells, including malignant tumors and blood cancers. Benign tumors and non-blood cancer leukemias are not cancers and can be cured through surgery or targeted drugs. However, malignant tumors and blood cancers cannot be cured through surgery and targeted drugs because the genomes of cancer cells are unstable, with descendants continuously mutating, spreading, metastasizing, and escaping immune destruction. Surgery can remove tumors but cannot remove cancer cells in the blood. Targeted drugs can kill targeted cancer cells and normal cells, but cannot kill non-targeted cancer cells and normal cells.
Taking the three most advanced classes of targeted drugs as an example, they are all the result of years of scientific research, including Nobel Prize winners. Why can't they cure diseases like cancer in humans?
From the patient's perspective, each patient's genomic DNA sequence is different. Genomic mutations vary from person to person. Their likelihood of developing common lesions or cancer is less than 1%.
From the drug's perspective, each drug has a specific structure and specific targets, which do not change for 10 or 100 years. However, patients with genomic mutation targets are rare. Each patient's genomic DNA sequence is different. Genomic mutations vary from person to person. Therefore, the population that benefits from a targeted drug is about 3%.
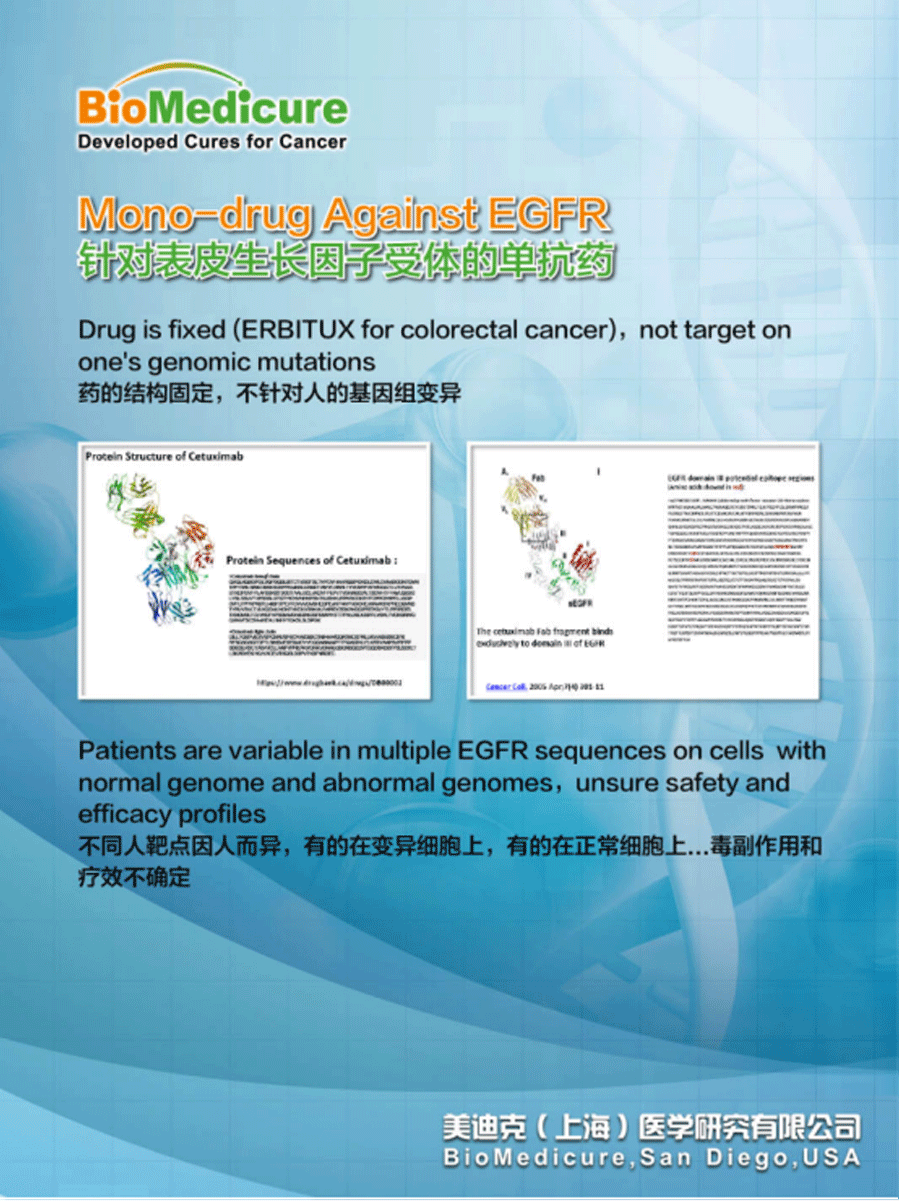
The limited efficacy of monoclonal antibody targeted drugs and the fundamental reason for good gene toxicity side effects is that they do not target new antigens, are not part of the immune system, and do not follow the natural laws of the immune system...
CAR-T cell therapy has chimeric antigen receptors that target chimeric antigens, but also do not target new antigens. Therefore, it similarly has uncertain efficacy and side effects.
Is it possible to customize a treatment based on genomic mutations that targets pre-antigens, specifically killing mutated cells, precancerous cells, and cancer cell populations without harming any normal cells? The answer is yes.


